
You need help with addiction. That part you know. But disappearing from your life for three months? Not happening. You've got a job that actually pays the bills. Kids who need you around. A lease with your name on it. This is where Outpatient Treatment helps. Outpatient drug and alcohol treatment in Tampa means you get professional help without disappearing. Therapy sessions happen mornings, evenings, weekends. Whatever fits your schedule. Then you head home. It's not some shortcut. Just treatment that actually fits into a real person's life.
Here's how outpatient treatment works: you live at home and show up for scheduled therapy sessions. Not like residential rehab where you're at a facility 24/7. You attend treatment, could be morning, afternoon, evening, weekend, and then you leave. Head back to your house, your apartment, wherever.
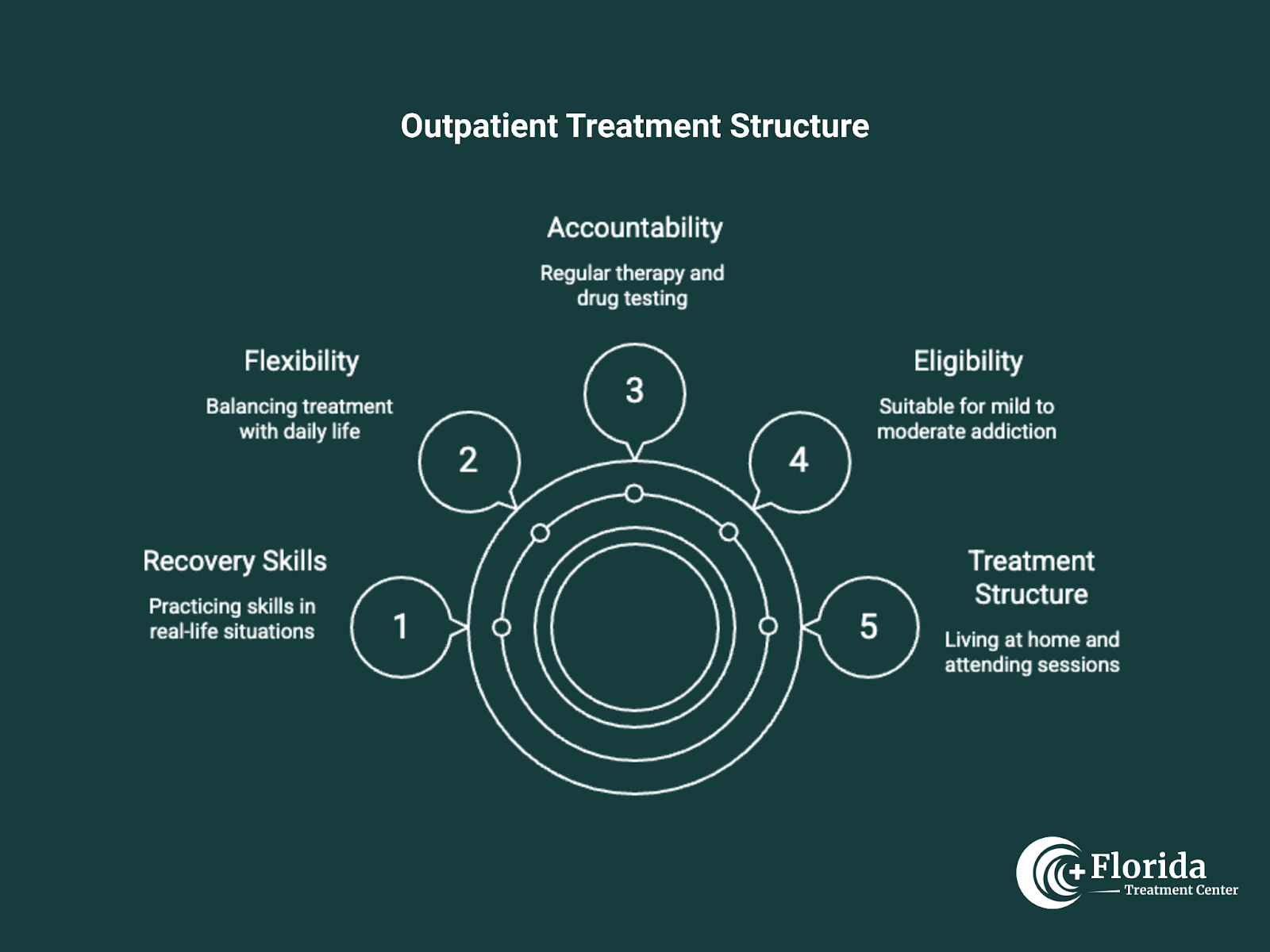
Who it's for:
Works well for people dealing with mild to moderate addiction who've made it through detox already. You need a stable place to sleep. Also good if you've finished inpatient care and you're ready for the next step down. Still need support, just done with full-time treatment.
The Balance:
Here's what you get: accountability. Regular therapy, drug testing, someone actually checking in. But also flexibility, work your job, go to class, pick your kids up from school, make it to their games. The real difference? You're practicing recovery skills while dealing with actual life. Real triggers. Real stress. The coworker who drives you nuts. Traffic on I-275. Bills stacking up. Whatever normally makes you want to use, it's all still there. But now you're figuring out how to handle it instead of avoiding everything in some bubble.
Where it fits:
Most people do detox first, maybe inpatient treatment, then step down to outpatient. That's the usual path. Makes sure you're getting enough support at each stage without keeping you in more intensive care than you actually need.
Tampa's growing fast. More people means more need for addiction treatment that doesn't force impossible choices. Can't take three months off work? Need to stay near your kids? Outpatient rehab in Tampa removes that barrier; you don't have to abandon your entire life to get help.
Staying local matters:
You keep your connections with family instead of disappearing to some facility in another county or state. You keep showing up to work or class. You deal with the actual triggers in your environment, the bar on your street corner, the friend who still uses, the stress from your specific job, instead of temporarily avoiding them. For parents especially, staying in Tampa means you're still there. Still picking kids up. Still helping with homework. Still being their parent while you're getting better.
After inpatient treatment:
Finished residential treatment somewhere? Tampa outpatient programs give you continued support during that weird, vulnerable time when you're back to regular life. You're not jumping from 24/7 care straight to complete independence. You get professional guidance while you're figuring out how to navigate everything again.
Tampa's recovery community:
Tampa has a solid recovery community. Plenty of 12-step meetings around the area. Carrollwood. South Tampa. Westchase. Brandon. Support groups. Sober activities. Our outpatient program connects you with all of it. Your support network goes way beyond just the formal treatment sessions.
Florida Treatment Center offers multiple levels of outpatient care. Start where you actually need to start. Move between levels as things change in your recovery.
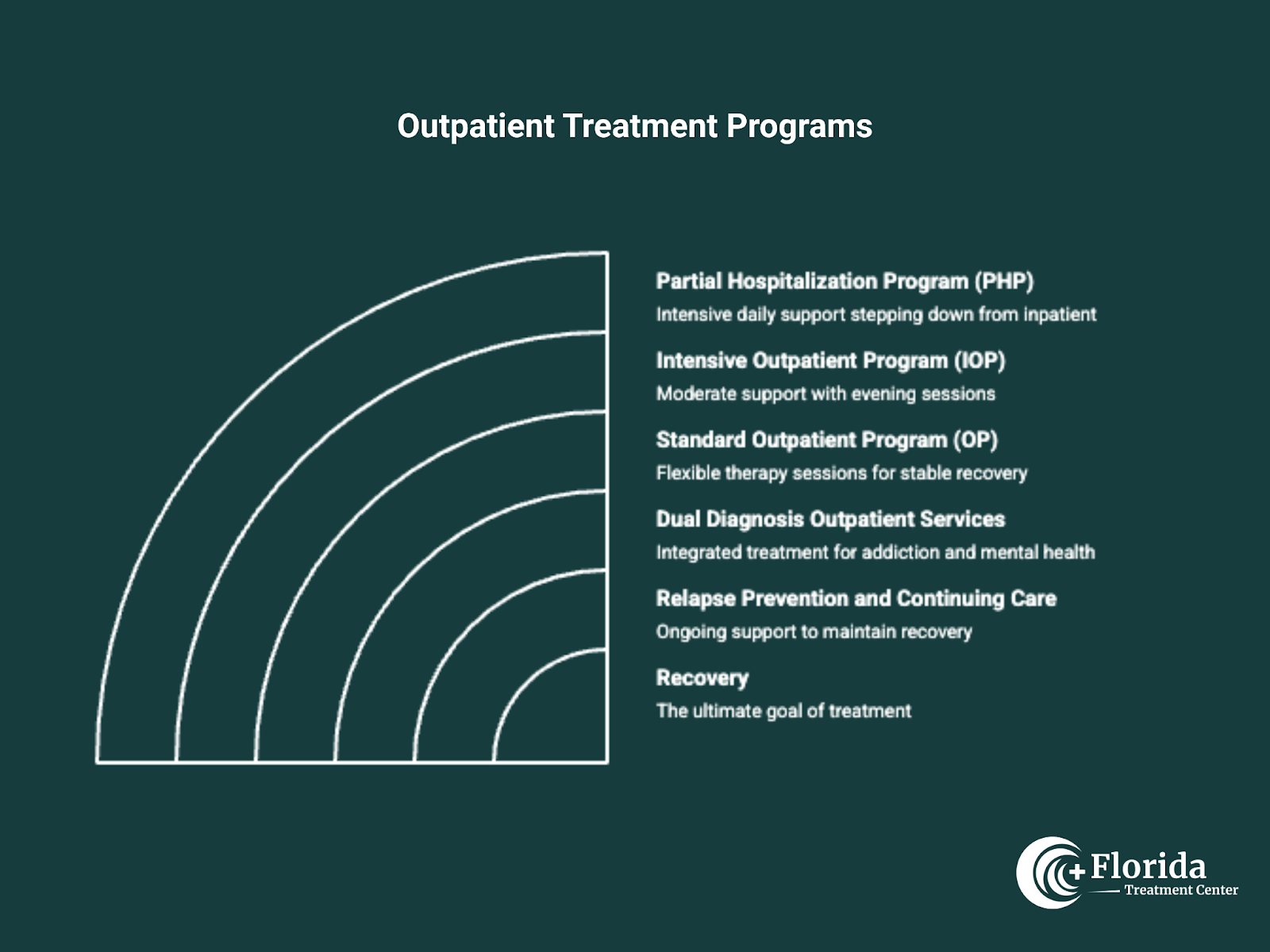
This is the most intensive outpatient level. You're showing up 5-7 days a week for several hours each day. Getting comprehensive clinical services, individual therapy, group counseling, psychiatric care, medication management if you need it. Then heading home each evening.
PHP makes sense if you're stepping down from inpatient and still need serious daily support. Or if things are serious enough that once-a-week therapy isn't sufficient, but you don't need hourly check-ins.
The middle ground. You meet 3-5 days a week, 3-4 hours per session. Often scheduled for evenings so your workday stays intact. Group therapy, individual counseling, family sessions, learning to prevent relapse.
Good fit if you're dealing with moderate substance use problems. Or if you're coming from PHP and need substantial ongoing support but not the full-day commitment anymore.
Most flexible option we've got. You're doing 1-3 therapy sessions weekly, mix of individual counseling, group therapy, family sessions. This is where you step down when you're showing real stability in early recovery but you're not ready to be completely on your own yet.
You've got most of your independence back. You're managing. Just need continued guidance to keep it that way.
Lot of people dealing with addiction also have depression. Or anxiety. PTSD. Other mental health stuff going on. Our dual diagnosis services tackle both things at the same time. Clinicians trained in addiction and mental health care working with you.
Because treating just the addiction while your mental health falls apart? That's setting you up for relapse later on.
Support doesn't end when treatment does. Regular check-ins happen. Maintenance groups. Alumni programming. Counselors available when things get difficult.
Initial assessment and personalized treatment plan:
You start with an assessment. We ask about your substance use history, mental health, living situation, who's in your corner, what you actually want out of treatment. Nobody's sitting there judging you. We're trying to understand your situation so we can build a plan that fits. Your treatment plan spells out the therapy approaches we'll use, how often you're coming in, specific goals you're working toward, how we're tracking progress. Nothing's locked in forever. Things change. The plan changes with you.
Evidence-based therapies used:
We use approaches that actually work. Research-backed stuff, not just whatever sounds good:
Peer support and family involvement:
Group therapy puts you in a room with people who get it because they're going through it too. Cuts down on the isolation and shame. You get practical advice from people who've been exactly where you are. Family therapy brings your loved ones into this. Addiction messes up relationships: partners, kids, parents, siblings, everyone. Family sessions work on fixing that damage. Teaching your family how to support you without enabling. Making your entire support system stronger.
Progress monitoring:
Your clinician tracks how you're doing through regular check-ins, drug testing, feedback from sessions. Struggling with something? We adjust. Add more support, increase how often you're coming in, try different approaches. Doing well? We step you down to less intensive care. You always get what you actually need. Not some cookie-cutter program that treats everyone exactly the same.
Core principles of addiction treatment apply across the board. But the specifics? They matter.
Key differences:
Alcohol withdrawal can actually kill you. So can withdrawal from opioids and benzos. Your outpatient program works with medical providers to make sure you're physically stable before or during treatment. This isn't optional. Triggers look completely different for alcohol versus drugs. Alcohol is legal. It's everywhere. Socially acceptable. You're trying to stay sober in a culture where everyone's grabbing drinks after work. Drug use usually involves different social circles, different ways of getting the substance, different legal problems. Treatment has to address these specific differences.
Specialized approaches:
For opioid addiction, we bring in medication-assisted treatment (MAT) pretty often. Buprenorphine or naltrexone paired with counseling. For alcohol, could be naltrexone or acamprosate. These meds aren't substitutes for the work. They just reduce cravings and withdrawal so you can actually concentrate in therapy and build real skills.
Stimulant addiction needs different approaches. Managing those intense cravings. Dealing with the mood crashes after you stop using. Cannabis treatment focuses on recognizing the dependency (because a lot of people don't think weed counts as addictive) and building other ways to cope with stress.
What works:
Outpatient treatment works. Research backs that up. How well it works depends on a few things. How long you stick with it. Whether you actually complete the program. How engaged you are. Your support system. Your motivation level. People who finish and stay connected to aftercare do way better than people who get no treatment or drop out early.
Transitioning from inpatient to outpatient care:
Finished residential treatment? Outpatient care keeps you connected as you're getting back to regular life. Going from 24/7 support straight to complete independence? That's usually a setup for failure. Outpatient gives you the middle ground, continued support while you're practicing what you learned in real-world situations. Your outpatient therapist helps you apply your skills to actual life problems. Addresses stuff as it comes up. You're not alone during those first vulnerable months.
Aftercare, community support, and ongoing therapy:
After you finish formal outpatient treatment, aftercare keeps you plugged in. Support group meetings. Alumni groups. Periodic check-ins with your counselor. Staying connected with people you met during treatment. Tampa's recovery community has a lot to offer. Volunteering opportunities. Sober activities. Connections with people who understand what you're dealing with because they've been there.
Rebuilding your life:
Outpatient treatment lets you rebuild while getting professional support when you need it. You learn to handle triggers as they actually happen. Not in theory, in real time. You rebuild trust with family through consistent actions, not promises. You figure out who you are when you're not using.
Happens gradually. With guidance available. You're building a life that's good enough you don't need to escape from it.
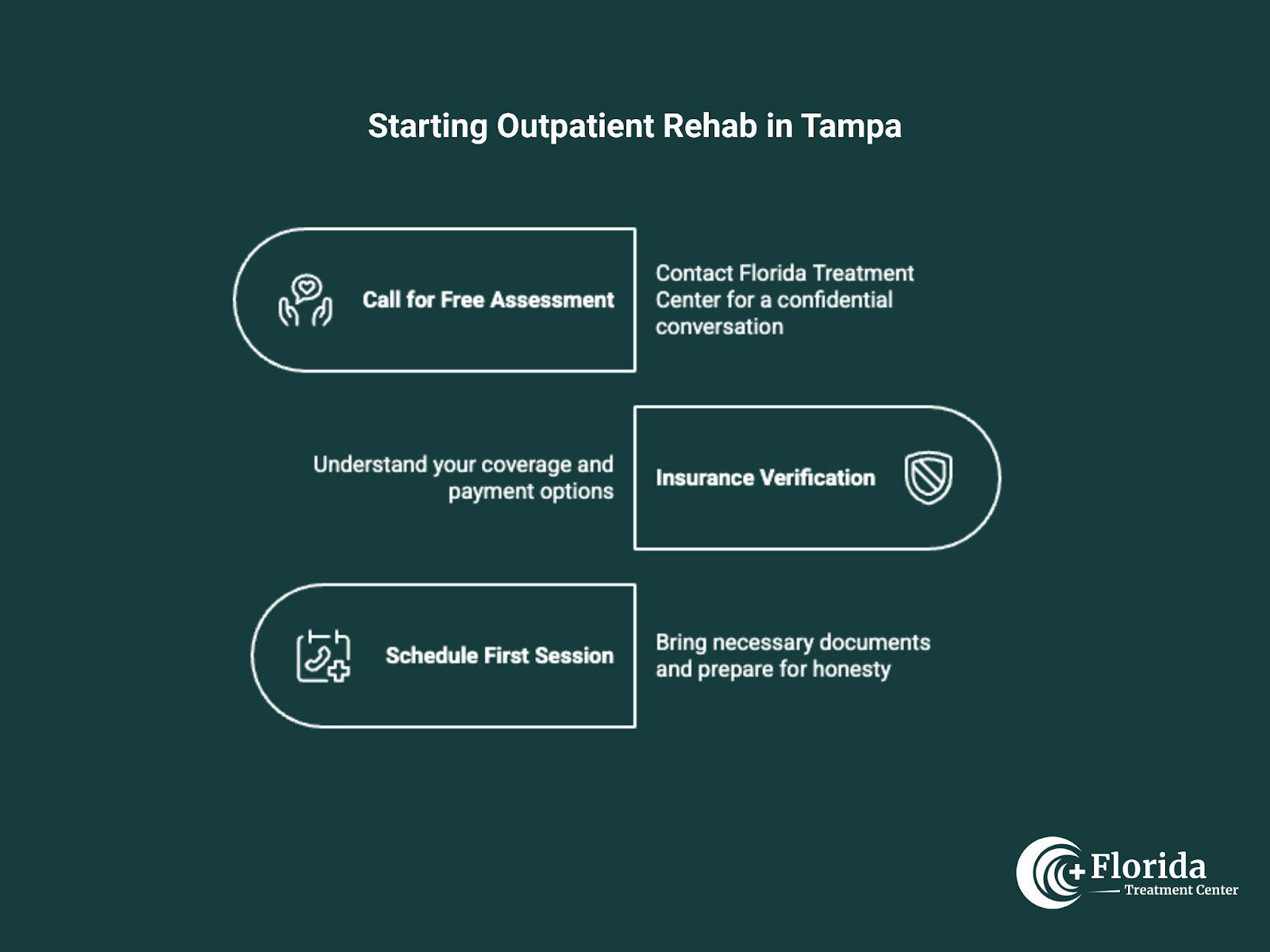
Getting started is pretty straightforward:
1. Call for a free assessment
Contact Florida Treatment Center. Have a confidential conversation about where you are and whether outpatient makes sense for you. No pressure. No judgment. Just an honest conversation about what you need.
2. Insurance verification
We work with most major insurance plans. We'll help you understand your coverage, explain any out-of-pocket costs, talk about payment options if you need them. Goal is getting rid of the barriers between you and getting help.
3. Schedule your first session
Bring your ID, insurance card, list of current medications, contact info for your healthcare providers. Show up ready to be honest about your situation, everything stays confidential.
Our clinicians have worked with people in your exact situation before. They understand what you're dealing with. They actually want to help.
Contact us:
Your recovery can start today. You don't need to wait until you hit rock bottom. Don't need everything figured out. If part of you is wondering whether it's time, that's probably your answer.
Call Florida Treatment Center:
Scheduling's flexible here. Evening sessions available. Weekend slots too. Keep your job. Stay connected to family. Handle what you need to handle. Get treatment that works. No need to figure this out alone.
Psychologists and psychiatrists both work in the mental health field, but they differ in their approaches. Psychologists primarily use talk therapy and counseling to address emotional and behavioral issues, while psychiatrists are medical doctors who can prescribe medication in addition to therapy.
Stay informed about the latest research in psychology.
IOP provides a higher level of care than standard outpatient , with more frequent therapy sessions and structured support.
PHP offers the most structured and intensive level of care while allowing clients to return home at the end of the day.